NEET SS Anaesthesia Exam Preparation Program

Our NEET SS Anaesthesia Preparation Program offers structured exam-oriented learning, high-yield clinical concepts, MCQ-based practice, and expert guidance to help aspirants achieve success in the NEET SS Anaesthesia examination.
This program provides systematic preparation strategies, syllabus-focused study plans, and practical exam techniques required to confidently attempt NEET SS Anaesthesia and secure a super-specialty seat
Overview of NEET SS Anaesthesia Preparation with Exam-Focused Learning
The NEET SS Anaesthesia Preparation Strategy delivers comprehensive learning through exam-pattern–based MCQs, concept-oriented notes, and applied clinical reasoning aligned with the latest NEET SS guidelines.
NEET SS Anaesthesia tests not only factual knowledge but also clinical judgment, interpretation, and decision-making skills essential for advanced anaesthesia practice. Structured preparation ensures clarity, consistency, and exam readiness.
Importance of Structured Preparation for NEET SS Anaesthesia
This preparation program emphasizes strong conceptual foundations combined with continuous MCQ practice, revision strategies, and performance analysis, ensuring focused and efficient exam preparation aligned with national examination standards.
A systematic approach helps candidates manage time, avoid common mistakes, and maximize scoring potential.
Core Preparation Syllabus & Focus Areas
High-yield topics covered in NEET SS Anaesthesia preparation include:
-
Airway management and difficult airway algorithms
-
Anaesthesia pharmacology and drug interactions
-
Anaesthesia machine, equipment, and monitoring
-
Cardiac, neuro, obstetric, and pediatric anaesthesia
-
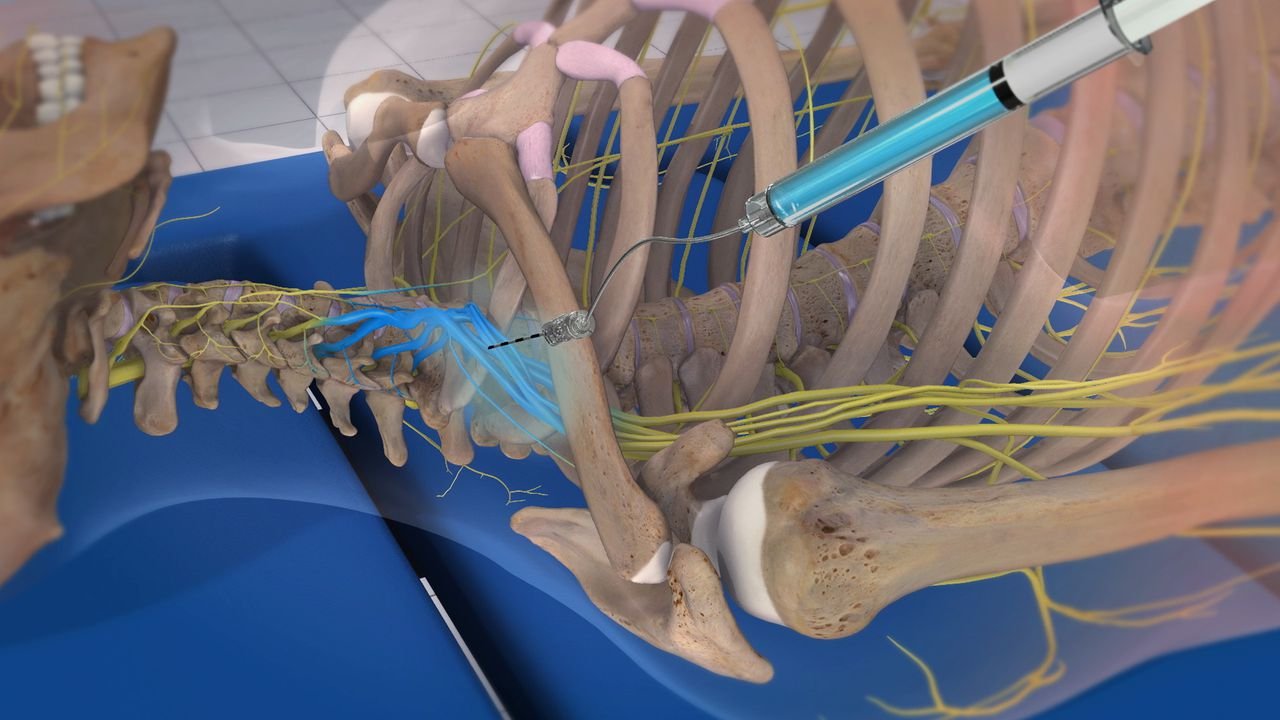
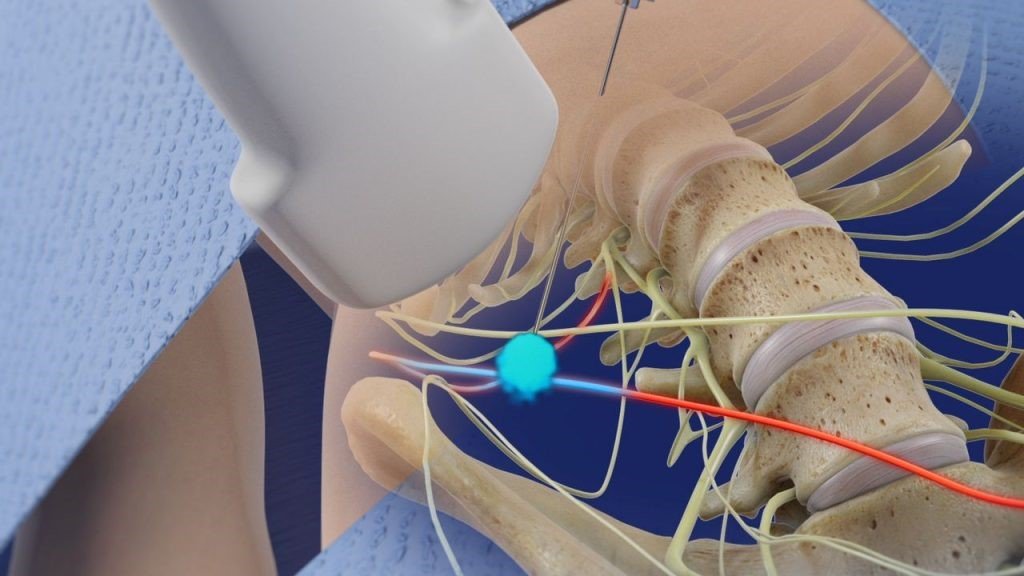
Regional anaesthesia: spinal, epidural, nerve blocks
-
Critical care, ICU management, and ventilation
-
Pain management and NORA
-
Applied physiology and perioperative risk assessment
Professional Preparation for NEET SS Anaesthesia Aspirants
This preparation program is designed for:
-
MD / DNB Anaesthesia candidates
-
Anaesthesia residents
-
Final-year postgraduate students
-
Practicing anaesthesiologists preparing for NEET SS
-
Doctors aiming for super-specialty anaesthesia training
Eligibility Criteria for NEET SS Anaesthesia Preparation
Eligibility for NEET SS Anaesthesia preparation includes:
-
Recognized postgraduate qualification in Anaesthesia (MD/DNB)
-
Valid medical registration
-
Basic clinical anaesthesia knowledge
-
Commitment to structured exam preparation
Benefits of NEET SS Anaesthesia Preparation Program
With increasing competition in NEET SS Anaesthesia, structured preparation offers:
-
Clear understanding of exam pattern and expectations
-
Improved accuracy and speed in MCQ solving
-
Strong clinical concept integration
-
Reduced exam stress through systematic revision
-
Better time management during the exam
-
Increased chances of securing a super-specialty seat
Advanced NEET SS Anaesthesia Exam Strategy
NEET SS Anaesthesia preparation equips aspirants with exam-smart techniques, concept clarity, and confidence required to perform under pressure.
A structured, guideline-aligned preparation strategy ensures consistent progress, professional growth, and success in NEET SS Anaesthesia.
Start Your NEET SS Anaesthesia Preparation Today
Focused learning, regular practice, and expert guidance are the keys to success in NEET SS Anaesthesia. Begin your preparation journey with a structured strategy designed to help you achieve your super-specialty goals.
“The structured NEET SS Anaesthesia preparation strategy helped me organize my study plan efficiently. The concept-oriented approach and MCQ practice significantly improved my confidence and accuracy.”
“This program made complex anaesthesia topics easy to understand. Regular practice questions and focused revision helped me stay consistent throughout my NEET SS preparation.”
“A well-structured and practical preparation plan. The MCQs and concept-based learning helped me identify weak areas and improve steadily before the exam.”
“This NEET SS Anaesthesia preparation strategy is perfect for serious aspirants. It balances theory, MCQs, and revision, making exam preparation more focused and effective.”